Introduction
Thyroid nodules are common, with studies suggesting that up to 50% of individuals may have them by the age of 60. While most nodules are benign, the potential for thyroid cancer raises important questions about diagnosis, management, and treatment. Understanding thyroid nodules involves exploring their types, diagnostic approaches, biopsy techniques, and available treatment options. This article aims to provide a comprehensive overview to help patients navigate the complexities of thyroid nodules effectively.
Understanding Thyroid Nodules
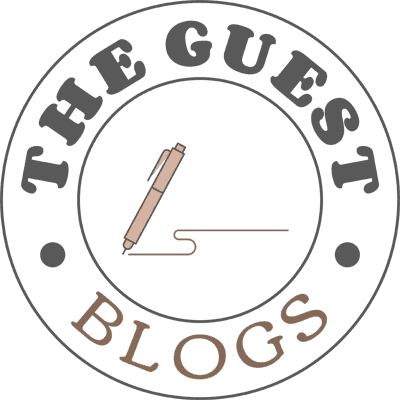
What Are Thyroid Nodules?
Thyroid nodules are abnormal growths within the thyroid gland, located at the base of the neck. The thyroid gland is responsible for producing hormones that regulate metabolism, energy production, and overall body functions. Nodules can vary in size, shape, and composition and can be solid or fluid-filled (cystic).
Types of Thyroid Nodules
- Benign Nodules: The majority of thyroid nodules are non-cancerous. Common benign types include:
- Colloid Nodules: Result from the overproduction of thyroid hormones and often do not cause symptoms.
- Follicular Adenomas: Solid nodules that may require monitoring due to a small risk of cancer.
- Thyroid Cysts: Fluid-filled sacs that typically do not require treatment unless they cause symptoms.
- Malignant Nodules: Thyroid cancer is less common but can occur. Types of thyroid cancer include:
- Papillary Thyroid Carcinoma: The most common type, often grows slowly and has a good prognosis.
- Follicular Thyroid Carcinoma: More aggressive than papillary cancer, requiring careful monitoring.
- Medullary Thyroid Carcinoma: Arises from C cells and may be associated with genetic syndromes.
- Anaplastic Thyroid Carcinoma: A rare, aggressive form that requires prompt treatment.
Prevalence and Risk Factors
Thyroid nodules can occur in anyone, but certain factors may increase the likelihood of developing them, including:
- Gender: Females are more likely than males to develop nodules.
- Age: The incidence of nodules increases with age.
- Family History: A family history of thyroid disease may elevate risk.
- Exposure to Radiation: Previous radiation therapy to the head or neck can increase the risk of nodules and thyroid cancer.
Diagnosing Thyroid Nodules
Initial Evaluation
The diagnosis of thyroid nodules begins with a thorough evaluation, including:
- Medical History: A healthcare provider will gather information about symptoms, family history, and risk factors.
- Physical Examination: The provider will palpate the thyroid gland to identify the presence of nodules and assess their size and consistency.
Imaging Studies
- Ultrasound: The primary imaging technique used to evaluate thyroid nodules is ultrasound. It helps in:
- Determining the size and composition (solid, cystic, or mixed) of the nodule.
- Assessing characteristics that may indicate malignancy, such as microcalcifications, irregular borders, and increased vascularity.
- Fine Needle Aspiration (FNA) Biopsy: If a nodule raises suspicion for cancer based on ultrasound findings, an FNA biopsy may be recommended. This procedure involves using a thin needle to extract cells from the nodule for cytological examination.
- Thyroid Scintigraphy: A nuclear medicine test that evaluates the functional status of the thyroid gland. It helps distinguish between “hot” nodules (which produce excess hormones and are usually benign) and “cold” nodules (which may require further evaluation).
Biopsy Techniques
Fine Needle Aspiration (FNA)
FNA is the most common method for obtaining tissue samples from thyroid nodules. The procedure involves:
- Preparation: The patient is positioned comfortably, and the skin over the nodule is cleaned.
- Anaesthesia: Local anaesthesia may be applied to minimise discomfort.
- Needle Insertion: A thin needle is inserted into the nodule under ultrasound guidance to collect a small sample of cells.
- Sample Processing: The obtained sample is sent to a pathologist for examination.
FNA is minimally invasive, usually performed on an outpatient basis, and carries a low risk of complications.
Interpreting Biopsy Results
Biopsy results can be categorised as follows:
- Benign: No signs of cancer, often leading to routine follow-up.
- Suspicious: Some atypical cells may be present, requiring further evaluation or repeat biopsy.
- Malignant: Confirmed thyroid cancer, necessitating treatment planning.
The Bethesda System for Reporting Thyroid Cytopathology (BSRTC) is commonly used to classify FNA results and guide management decisions.
Treatment Choices for Thyroid Nodules
Monitoring and Observation
In cases where thyroid nodules are diagnosed as benign and asymptomatic, healthcare providers may recommend a conservative approach involving regular monitoring. This includes:
- Ultrasound Follow-Up: Routine ultrasound evaluations to monitor nodule size and any changes over time.
- Clinical Assessment: Periodic physical examinations to assess for new symptoms or changes in the nodule.
Surgical Intervention
- Malignant Nodules: If cancer is confirmed, surgical intervention is necessary.
- Suspicious Nodules: If FNA results are indeterminate or suspicious for cancer, surgery may be warranted.
- Symptomatic Nodules: Large nodules causing discomfort, difficulty swallowing, or cosmetic concerns may require surgical removal.
Types of Surgery
- Thyroid Lobectomy: Removal of one lobe of the thyroid gland, often performed for benign nodules or localised cancer.
- Total Thyroidectomy: Complete removal of the thyroid gland, typically indicated for malignant nodules, especially in cases of thyroid cancer.
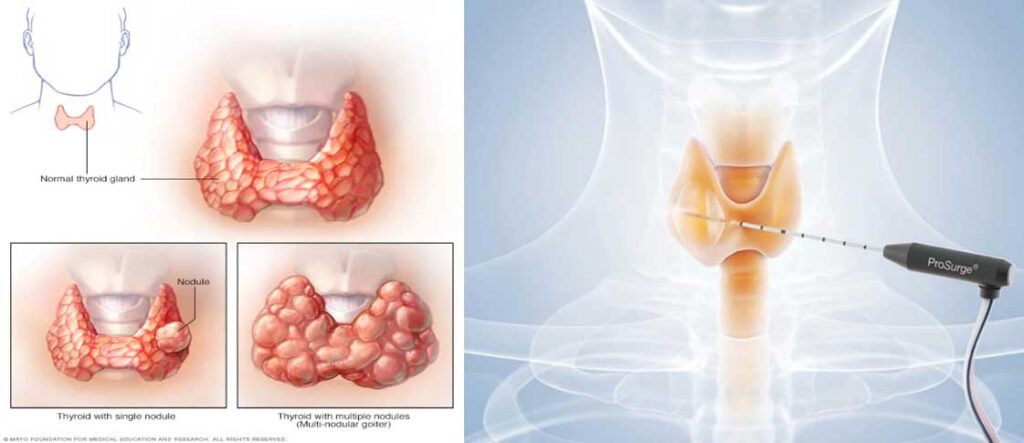
Microwave Ablation for Benign Thyroid Nodules
For benign thyroid nodules that require intervention due to size, symptoms, or cosmetic concerns, Microwave Ablation (MWA) is an effective, minimally invasive treatment option. MWA uses targeted heat to shrink the nodule, offering a non-surgical solution that preserves thyroid function. Here’s what you can expect in the treatment process:
Treatment Process:
-
Preparation: The procedure is typically performed under local anesthesia to ensure the patient’s comfort. A fine needle is inserted into the nodule, guided by ultrasound imaging, allowing precise targeting of the tissue.
-
Ablation: High-frequency microwave energy is delivered to the nodule, causing the tissue to heat up and shrink. This process is quick, typically taking between 20-30 minutes, depending on the size of the nodule.
-
Post-Treatment Care: After the procedure, patients may experience mild swelling or discomfort, which usually resolves within a few days. Patients are typically able to resume normal activities within a short recovery period.
Benefits:
-
Minimally Invasive: Unlike surgery, MWA doesn’t require incisions and leaves no scars.
-
Quick Recovery: Most patients experience minimal downtime, allowing them to return to daily activities quickly.
-
Effective in Symptom Relief: MWA significantly reduces the size of the nodule and alleviates symptoms like difficulty swallowing or visible neck bulges.
Follow-Up and Monitoring: To ensure the procedure’s success and monitor for any changes, follow-up is essential:
-
Ultrasound Monitoring: Regular post-treatment ultrasounds are used to track the nodule’s size and assess the effectiveness of the ablation.
-
Clinical Assessment: Routine check-ups allow the healthcare provider to evaluate for any recurrence of symptoms or complications.
Radioactive Iodine Therapy
For certain types of thyroid cancer, particularly well-differentiated thyroid cancers, radioactive iodine therapy may be used following surgery. This treatment involves administering radioactive iodine to destroy remaining cancerous thyroid cells and reduce the risk of recurrence.
Hormone Replacement Therapy
After surgical removal of the thyroid gland, patients may require thyroid hormone replacement therapy to maintain normal metabolic function. This involves taking synthetic thyroid hormone (levothyroxine) to ensure appropriate hormone levels in the body.
Conclusion
Thyroid nodules are a common clinical finding that requires careful evaluation and management. Understanding the diagnostic process, including imaging and biopsy techniques, is crucial for patients navigating their options. While most nodules are benign, the potential for malignancy necessitates a thoughtful approach to treatment.
Patients should work closely with their healthcare providers to determine the most appropriate management strategy based on individual risk factors, nodule characteristics, and personal preferences.